1. Excludes 1 Notes
According to the CDC, if two ICD-10-CM diagnoses are not related to each other, but they exist at the same time, they may both be reported together despite an Excludes1 note.
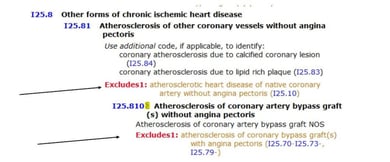
Originally, excludes1 advice stated that two codes could never be reported together. For example, review codes I25.10 for CAD of native vessels without angina and I25.810 for CAD of bypass grafts without angina. The tabular Excludes1 note at code I25.81- excludes code I25.10 CAD of native coronary artery w/o angina. This technically means that both cannot be reported together even though a patient could potentially have both.
We confirmed with the AHA that coders are to code both if present.
Another point of confusion is excludes1 notes and intestinal obstruction. For example, if a patient has stage IV colon cancer with bowel obstruction, can bowel obstruction be coded as principal or secondary diagnosis?
Per the notation at K56.6-, assign only the code for the carcinoma of the colon. No code would be assigned for any associated bowel obstruction. Impacts DRG as CC.
2. Diagnoses and “With” Subterms
The word “with” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index, or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List.
These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated. For conditions not specifically linked by these relational terms in the classification, provider documentation must link the conditions in order to code them as related.
Diabetes examples with:
-
-
- arthropathy NEC E11.618
- cataract E11.36
- chronic kidney disease E11.22
- circulatory complication NEC E11.59
- skin complication NEC E11.628
- HIA has written to AHA to define what the term “skin complication” should be interpreted as. For example, if a patient has cellulitis of the right foot and diabetes, should the case be linked and E11.828 be coded along with L03.115 or is the link not assumed?
-
Hypertension in a patient with CHF:
-
-
-
- I11.0, Hypertensive heart disease with heart failure
- Use additional code to identify type of heart failure (I50.-)
- I11.0, Hypertensive heart disease with heart failure
-
-
3. COPD Exacerbation with Pneumonia
Per Coding Clinic 3Q2016 page 15, assign J44.0, COPD with acute lower respiratory infection first, followed by code for pneumonia such as J18.9, Pneumonia, NOS.
This issue causes DRG assignment problems in that a patient admitted for treatment of pneumonia, will not be assigned to a pneumonia DRG if the patient has COPD.
Acute lower respiratory infection does not include “influenza” per CC3Q2016 page 16 as “influenza involves both upper and lower respiratory infection.”
-
-
- J18.9, Pneumonia as PDX
- J44.0, COPD with acute upper respiratory infection
- DRG 194, Simple pneumonia and pleurisy with CC
- Relative Weight: 0.9469
- J44.0, COPD with acute upper respiratory infection
- J18.9, Pneumonia as PDX
-
- J44.0, COPD with acute upper respiratory infection as PDX
- J18.9, Pneumonia (MCC)
- DRG 190, COPD with MCC
- Relative Weight: 1.1481
- What if the patient has aspiration pneumonia, J69.0 and COPD?
- Recommendation per Coding Clinic 1Q 2017 page 24 is that the note under J44.0 does NOT apply to J69.0, Aspiration pneumonia. Assign J44.9, COPD unspecified and J69.0, aspiration pneumonia. Either condition can be sequenced as principal diagnosis depending on the circumstances of admission.
- J18.9, Pneumonia (MCC)
- J44.0, COPD with acute upper respiratory infection as PDX
-
Keep in mind that on October 1, 2017, the “Use additional code to identify infection” note will change to “code also to identify infection” which has no sequencing guidance. So the above directives would be moot.
The information contained in this coding advice is valid at the time of posting. Readers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.






Leave a Comment