


Coding for treatment of cerebral aneurysms may...
With the implementation of ICD-10-CM came more...

It is difficult for coders to know when to report...

Health Information Associates (HIA), known for...

Fetal positioning within the uterus is not of...
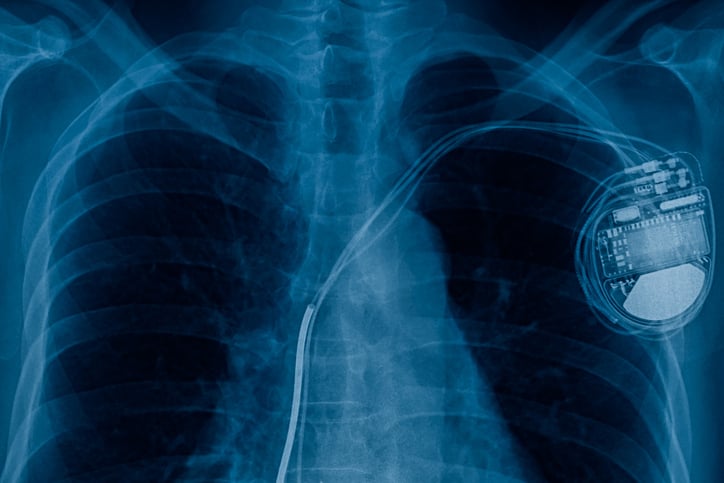
ICD-10-CM Code Z95.0 and Z45.018

A common misconception among coders is that...

Medicare Advantage Plans (Medicare part C) use...


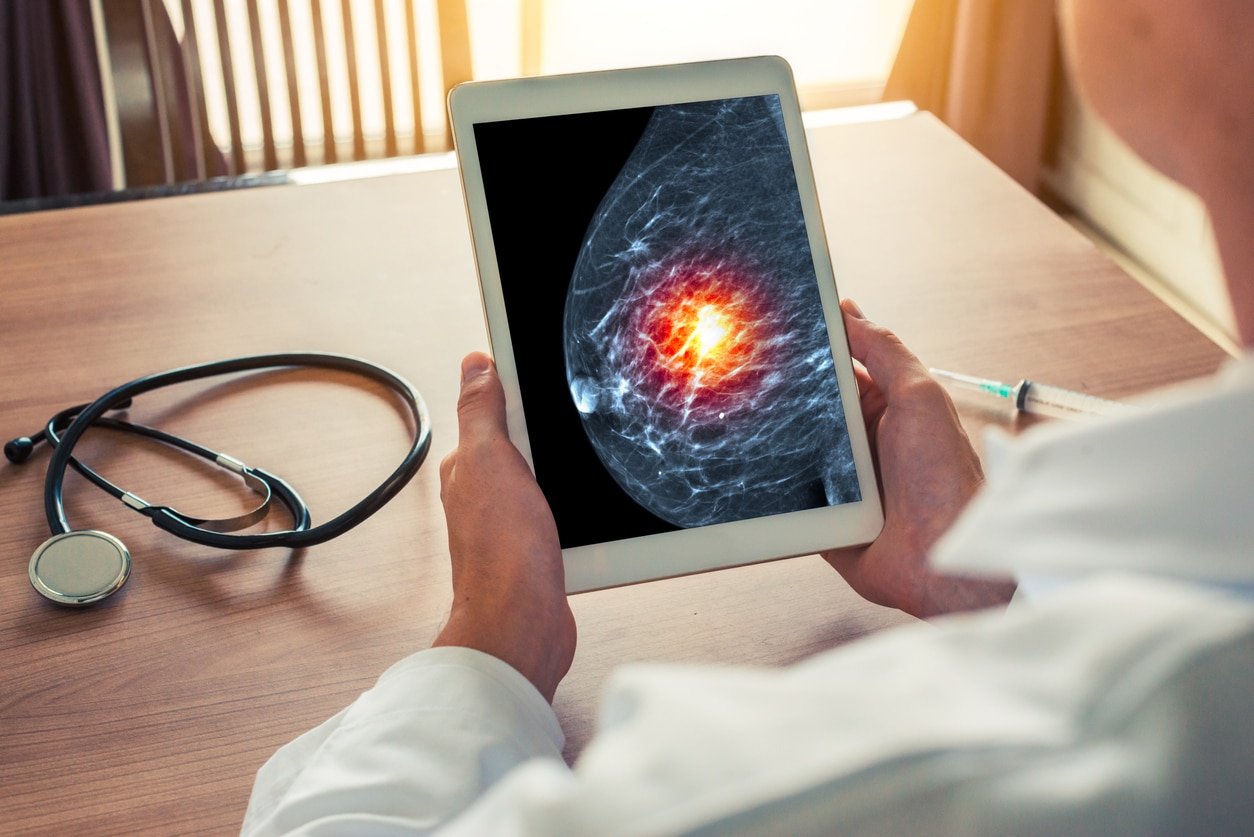
This coding tip provides an overview of coding...


Queries written in a multiple-choice format...

Hierarchical Condition Categories (HCCs) which is...


As you know, CMS and the CDC release the majority...

In this Coding Tip, we present the new ICD-10-PCS...


For FY 2024, the Official Guidelines for Coding...

Many coders who are coding obstetric cases are...

Anticoagulants and antiplatelets are used for the...

With the implementation of ICD-10-CM came...
In recent audit cases, HIA has seen coders...

This coding tip is intended to clear up any...

One of the issues addressed in AHA Coding Clinic®...

The focus of this coding tip is on the excision...

HIM and coding professionals may remember way...


HIA has found on Quality reviews that coders may...




This week’s coding tip focuses on the root...

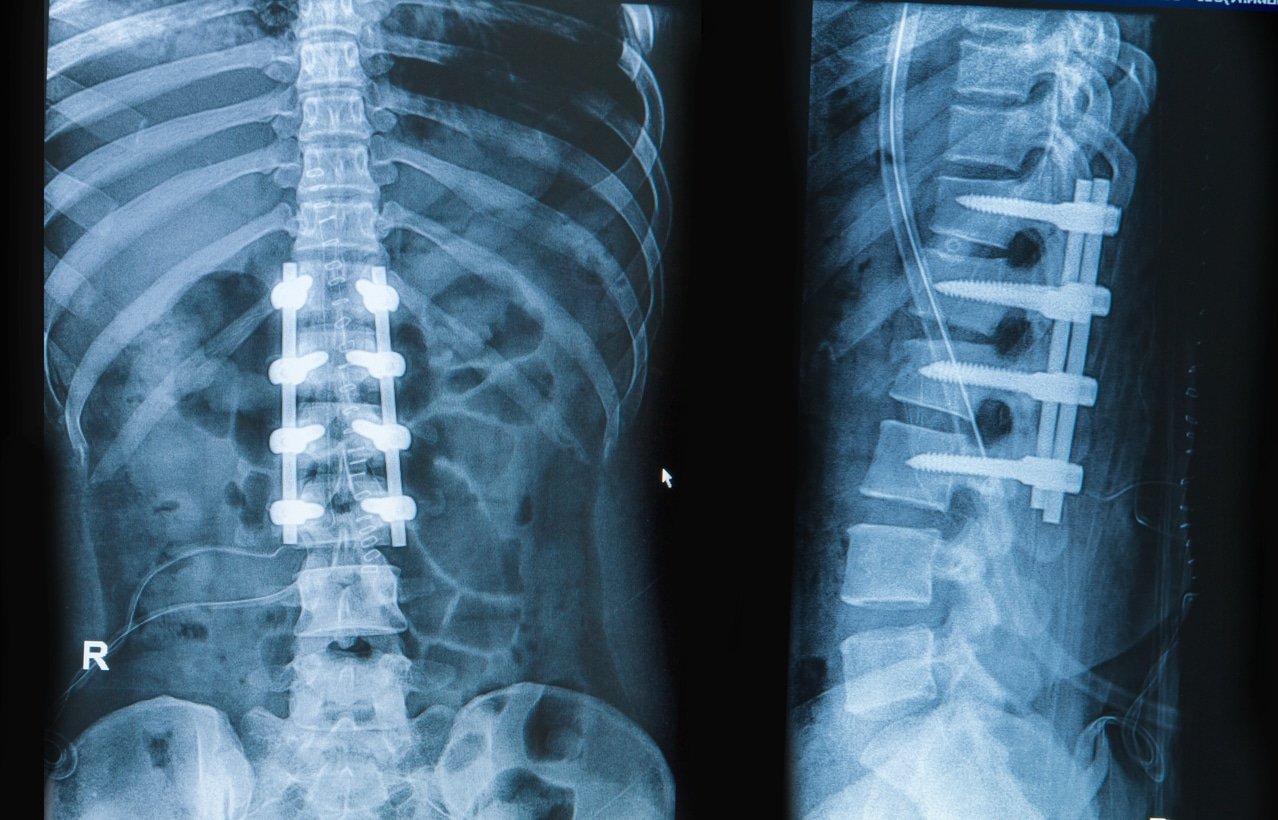
During a recent review of spinal fusion...
This week our focus is on the sequencing of the...

One of the most common mistakes that medical...

Social determinants of health,...

When coding interventional radiology, it can be...

Coding colonoscopies with multiple biopsies and...

Each year, CMS updates the National Correct...

This is a summary of the new CPT codes and HOPPS...

Some of our clients have received denials on...

In the healthcare industry, quality measures are...

As a coder, you may wonder why it is so important...

During some of our recent coding reviews, we have...


As coders, we see physicians document “elevated...

In the realm of medical coding, experience...

Medical coding errors are not just simple typos;...

Tissue findings interpreted by a pathologist are...

Medical coding audits are essential for...

Let's look at the different types of abuse,...

Medical coding audits are crucial to ensuring...

It is that time of year again where the new codes...


August marks Ambulatory Surgery Center Month, a...


Drug and alcohol use continues to rise in the...

As a coder, how often do you worry about meeting...

As more patients are being treated at home and as...

Most coders have probably noticed a rise in the...

How do coders report uncontrolled DM in ICD-10-CM?


Medical coding audits ensure the accuracy,...

The latest edition of AHA, Coding Clinic for...
Avoiding common mistakes during medical coding...


How can HIAlearn help close skills gaps across...

Several factors can contribute to the struggle of...

When Coding Departments are not running smoothly,...

Denial mismanagement can lead to financial loss,...


There are several reasons why you might want to...

Patients being admitted for acute renal failure...

If you're looking to move away from spreadsheets...

To make your medical coding audit budget go...

Partnering with a quality coding consulting...

So you failed your last medical coding audit, now...
HIA recently announced its internal Learning...

On December 21, CMS released the following...

HIA presents The 12 Pains of Christmas in ICD-10...


Health Information Associates (HIA) is proud to...

Coding audits can help target and address...

When Coding Departments are not running smoothly,...

New Technology Add-On Payments (NTAP) for 2023
In...

IPPS Changes for FY2023
In the previous two parts...

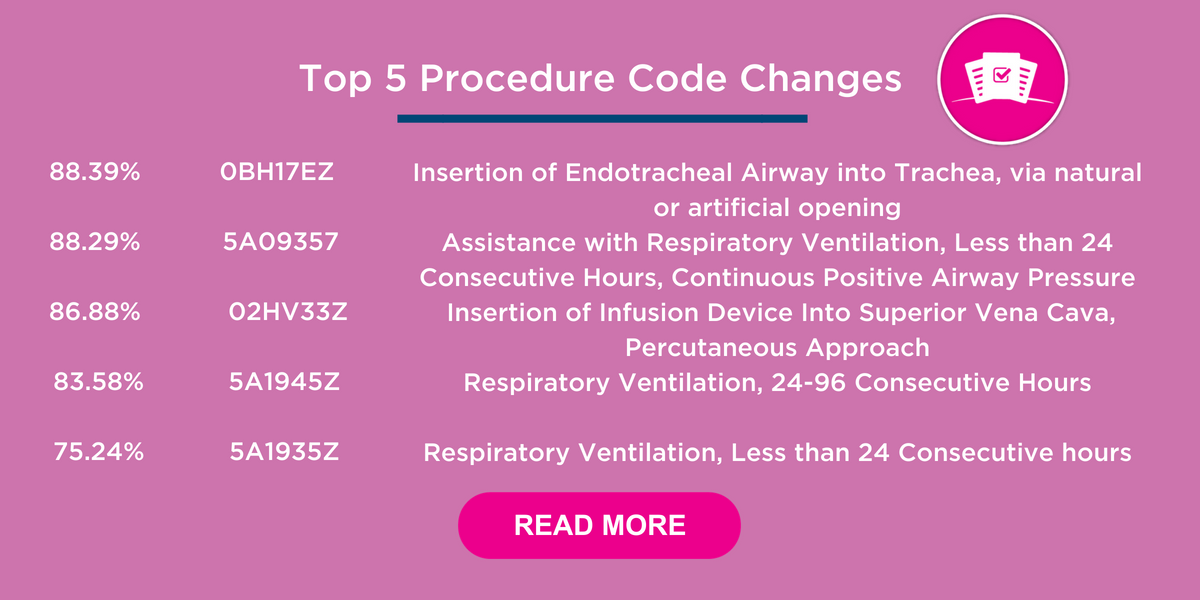
ICD-10-PCS Procedure Code Changes
This is Part 2...

This is Part 1 of a 4-part series on the 2023...


Selecting the Appropriate Root Operation –...







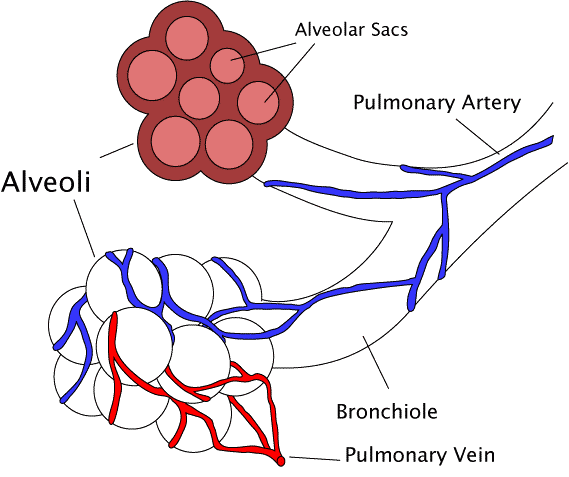
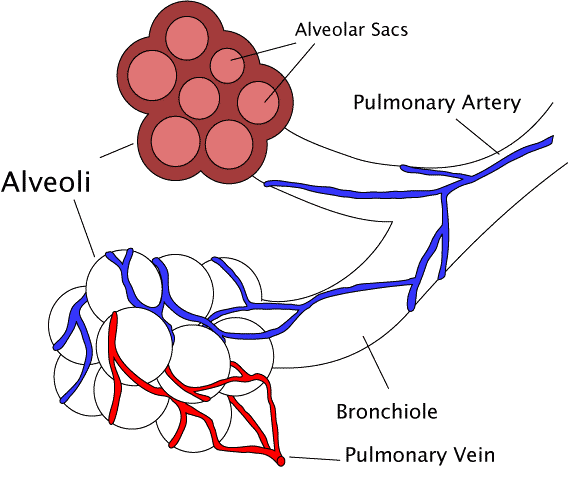
What is COPD?
COPD is a respiratory condition...



What is Pulmonary Hypertension?
Pulmonary...

How do coders report diabetic ketoacidosis in...

Reporting Endarterectomy in addition to the...

What is Clostridium Difficile Enterocolitis?
...

What is Alzheimer’s disease?
Alzheimer’s is a...

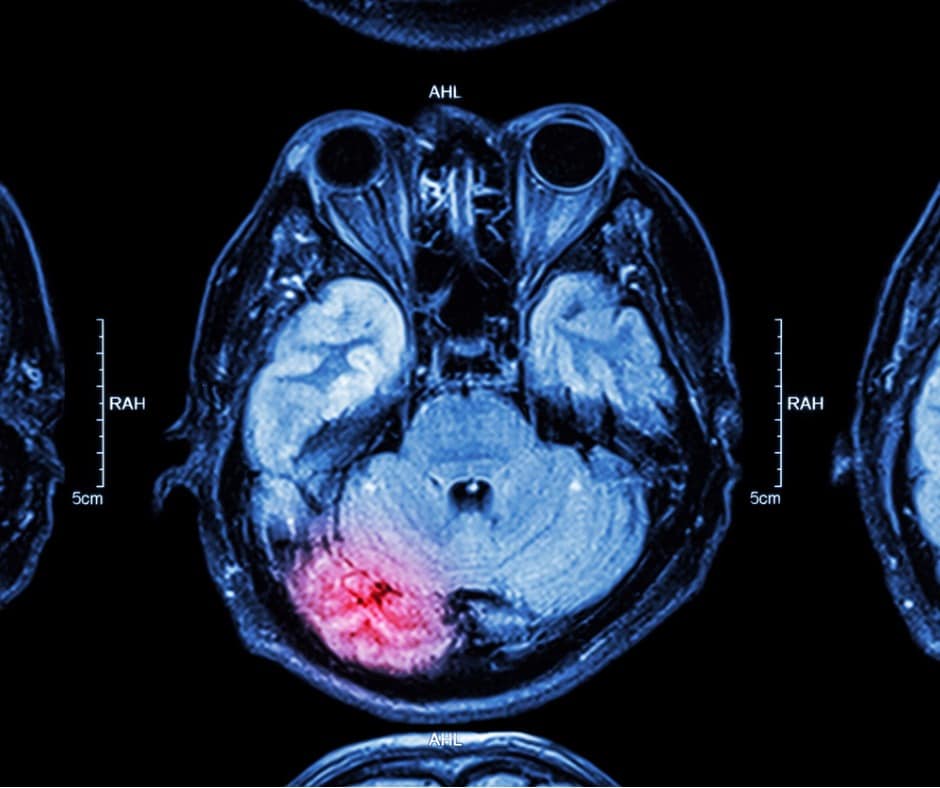
Cerebral Infarction Definition


Primary Diagnosis for Colonoscopy Records
Coding...


Below are some definitions for clarification:
...

Diagnoses in the Outpatient Setting


What is the Impella® external heart assist device?

In ICD-10-CM when comparative/contrasting...

When is it appropriate to report pleural effusion...

Pulmonary emboli are blood clots within the...

Wow, have you seen the proposed rule for FY2023...

Hospitals are receiving more inpatient denials...

HIA reviewed almost 50,000 inpatient...
This is the next most common DRG with...
This is the next most common DRG with...
This is the next most common DRG with...
This is the next most common DRG with...
This is the next most common DRG with...

As of April 1, 2022 discharges, the following...
This is the next most common DRG with...

This is the next most common DRG with...
This is the next most common DRG with...
HIA reviewed almost 50,000 inpatient...

This is Part 5 of a five part series on...

This is Part 4 of a 5-part series on the...

This is Part 3 of a 5 part series on the...

This is Part 2 of a 5 part series on the...

This is Part 1 of a five part series on...


I attended the 2022 CPT Symposium and...

Did you get a chance to read the FY2022...

In the previous three parts of this...

In the previous two parts of this four...
Coders are instructed, at this time, to follow...

This is Part 2 of a 4 part series on the...

This is Part 1 of a 4 part series on the...

Hypercoagulable states are blood disorders that...

Encephalopathy is a general term and means brain...

Spinal procedure coding can be daunting for...
In June CMS released the final ICD-10-PCS...

It is that time of year! CMS released the IPPS...

From coding audit type to budget, here’s...
Superman ICD 10 Code
...

Practices have not seen many revisions to...

The latest edition of AHA, Coding Clinic for...

This is Part 5 of a five part series on...

This is Part 4 of a five part series on...

This is Part 3 of a five part series on...

This is Part 2 of a five part series on...

With the proliferation of COVID-19 cases, we...

Updates as of 1/01/21:
As you may know, assigning...

Updates from 1/19/21 in green font.

This is Part 1 of a five part series...
It’s been a crazy year (to say the...

We have seen many updates and changes to COVID-19...

In the previous three parts of this...

In the previous two parts of this four...

This is Part 2 of a 4 part series on the...

Reading the latest coding advice from AHA Coding...
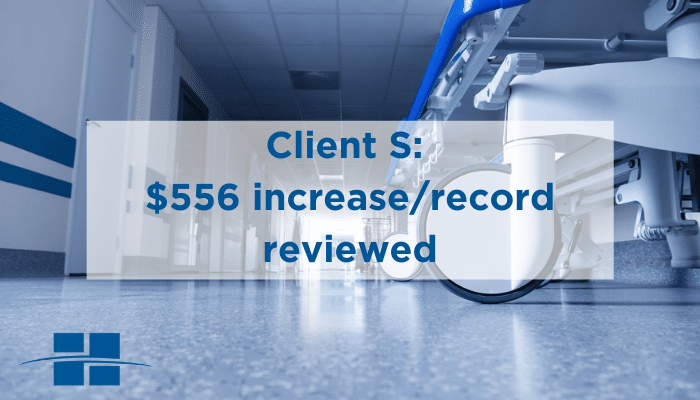
Let’s talk numbers.
“Client S” is a...
“Client X” is a not-for-profit, fully...


The Centers for Medicare and Medicaid...

Why are so many AKI records being...

Is the diagnosis clearly documented without...

Common Clinical Indicators for Acute Kidney...


There are several...

What is Acute Kidney Injury?
The terminology...

On March 6, CMS lifted some restrictions...


What to Know About Telehealth During the...

Companies around the world have told...
This is the final part of a three part...
This is part two of a three part series...
This is part one of a three part series...

In 2019, HIA reviewed over 725,600...

In 2019, HIA reviewed over 725,600...

In 2019, HIA reviewed over 725,600...

In 2019, HIA reviewed over 725,600...



CAUTION: The below applies for discharges...

We’re finally at the #1 most common DRG...

We’re now at the second most common DRG...
As stated in yesterday’s coding tip, HIA...

In 2019, HIA reviewed over 50,000...


In 2019, we reviewed over 50,000...

In 2019, we reviewed over 50,000...
In 2019, we reviewed over 50,000...

This is Part 5 of a five part series on...

This is Part 4 of a five part series on...

This is Part 3 of a five part series on...

This is Part 2 of a five part series on...
This is Part 1 of a five part series on...

Revision surgery on a reconstructed breast is...

There are two ways reconstruction with a tissue...
In some cases of breast implant...

In order to assign the appropriate CPT code for...

Changes in Cardiac Catheterization Code...


’Tis the holiday season—a time to...


Are Clinical Indicators Present to Support a...

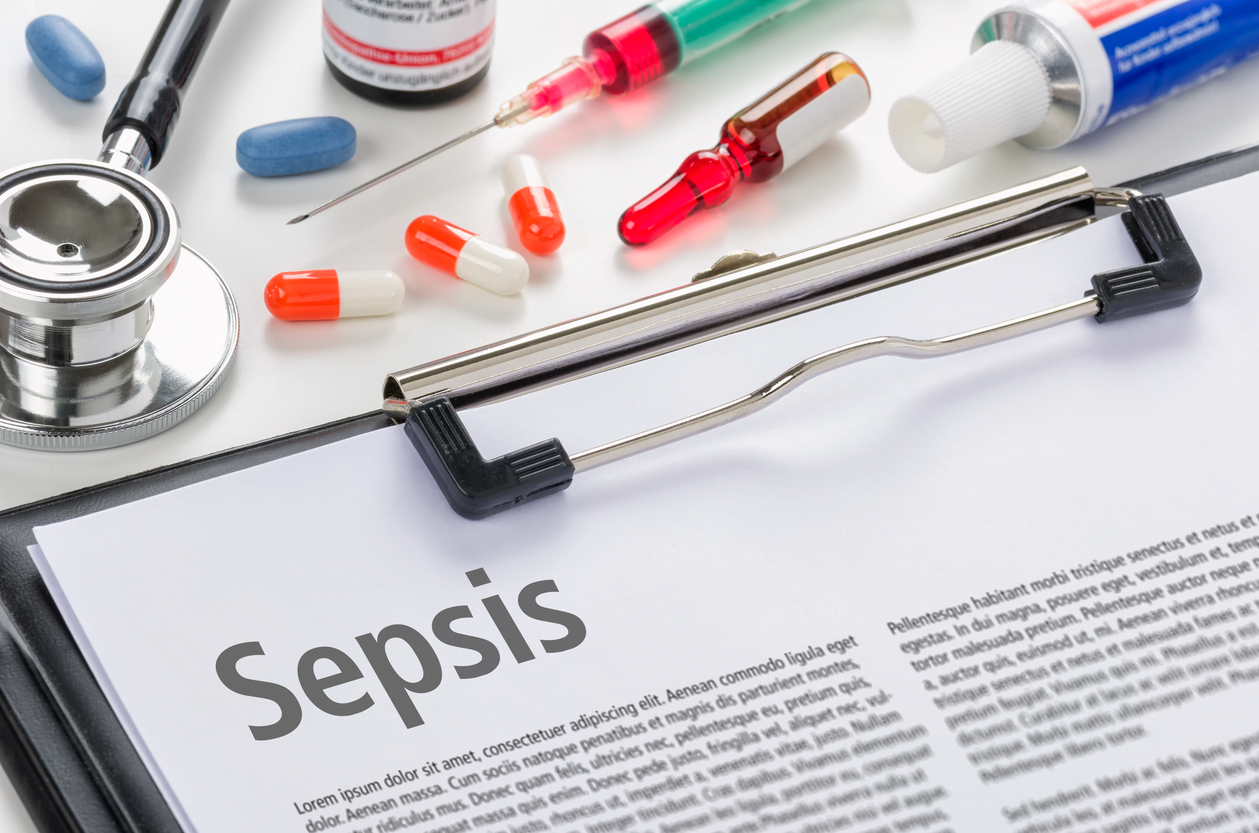
What is Severe Sepsis?
Severe sepsis occurs when...

Sepsis Sequencing
Sepsis can be caused by many...


New Technology Add-On Payments (NTAP)-...


New ICD-10-CM Codes
In Part 1 of this 4...

New ICD-10-CM Codes
This is Part 1 of...

Spinal Fusion Series Summary
Most common...

Harvesting of the autograft for spinal fusion—is...
What is intra-operative peripheral neuro...

Computer assisted navigation is often used during...
Coders should be able to determine if a previous...

What does decompression mean when performed in...

What is a discectomy?
A discectomy is...

When performing a spinal fusion, the...


Health Information Associates...




Spinal fusion coding is a tough job for coders....




We have a case where the...
AHIMA19: Health Data and Information...

This patient is noted to...

What is the proper complication code...



Is a newborn at 40 weeks 0 day...



Question:
A patient was admitted for...


Smooth Sailing Ahead
JULY 28 – 31, 2019...
STRATEGIES FOR SUCCESS: IT STARTS WITH US

EMPOWERING PATIENTS, BREAKING BOUNDARIES,...


2019 WSHIMA Annual Meeting
MAY 17-18, 2019




Happy National Volunteer Week! This week...

“With highly complex rules and...

Pitfalls of unbundling and Modifier 59...







Cathy Casella Wyatt Human Resources...










2019 Annual CHIMA Meeting
MAY 2-3, 2019...




2019 Quad-State Annual Meeting
MAY 5-8,...

ASCA 2019 Conference & Expo
MAY 15-19,...

2019 Annual CHIMA Meeting
MAY 2-3, 2019...


Happy New Year!
Every year, we...

2019 Annual ILHIMA Meeting
APRIL 25-26,...
2019 MOHIMA Annual Meeting
APRIL 3-5, 2019
OHIMA’s 2019 Annual Meeting
MARCH 18-20,...


Definitions/Explanations...



In order for coders to correctly report the use...

Bronchoscopy with Removal of Mucus Plugs or...

The rules about coding probable, possible and...

Chronic kidney disease (CKD) is the gradual loss...

Procedure code assignment for excisional...


In order for coders to correctly report the use...

On December 1, 2018, the HIA team...






“The biggest victims are the providers.”...



Pat Maccariella‑Hafey RHIA, CDIP, CCS,...



GHIMA 2018
AUGUST 19-20, 2018 PINE...

As seen in AHIMA’s August 2018 edition of...

CMS issues final rule, gives patients...

Looking for a fresh approach? Here’s how...
In this current, ever-changing healthcare...

Step into New Dimensions
JULY 29 – AUGUST...
What should a coder do in this scenario? Patient...

Pat Maccariella‑Hafey RHIA, CDIP, CCS,...
Pat Maccariella‑Hafey RHIA, CDIP, CCS,...

Pat Maccariella‑Hafey RHIA, CDIP, CCS,...

As Seen in the Journal of AHIMA. Who...

Having an Impact
MAY 1-4, 2018 | DURHAM,...

MAHIMA 2018
JUNE 10-12, 2018 SEACREST...

HIM: THE NEW FRONTIER
JUNE 2 – JUNE 6,...


Kim Carrier RHIT, CDIP, CCS, CCS-P...

New Technology-ICD-10-PCS Section “X” DRUGS
...




Joyce Will RHIT, CDIP, CPC, CPCO,...
25 Days of ICD-10 Christmas Calamity
’Tis...
25 Days of ICD-10 Christmas Calamity
’Tis...


Is Cellulitis always a skin complication of...

Other Heart Failure Coding
For FY2018 there is a...

Other Heart Failure Coding
For FY2018 there is a...

Partnering with HIA for Interim Auditing ...

“We have one final surprise tonight – and...
In order to assign the correct ICD-10-PCS code,...


Road to the 2017 AHIMA Conference
All...

Partnering with HIA for Interim Auditing...

Stress getting to you? Is stress making you...





Six Tips for Not Regretting your upcoming July...

Health Information Associates celebrates...
Patti Kulp RHIA, CSS, CDIP Review...

In this coding tip, we discuss the proper...

Below, Kim answers questions and offers her...

One of the updates to the ICD-10-CM Official...

Deborah Johnson MMHC, M.Ed., CHC,...

In ICD-10-PCS two codes are required to...

A capsule endoscopy is less invasive than the...


Biopsies are coded to the root operations...

Advanced Practice Provider (APP)...

4th Quarter 2016 Wellness Challenge Connects...


Please see the following post for the most recent...


Viral Sepsis is defined as a systemic infection...

Subscribe to our Newsletter
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.
Your previous visited blogs
Debridement is the medical removal of dead, damaged, or infe...
Coding for treatment of cerebral aneurysms may seem a little...
With the implementation of ICD-10-CM came more codes for rep...
It is difficult for coders to know when to report a symptom ...

